 Running on Empty: A Science-Based Solution for Sustainable Healthcare Leadership
Running on Empty: A Science-Based Solution for Sustainable Healthcare Leadership
By Traci Fisher, CEO
The Wellness Coach
Running on Empty
A scalpel moves with precision. The neurosurgeon's hands are steady, but her body is running on caffeine and adrenaline, five hours deep into a shift with no break.
An ER physician makes a life-saving call, though his nervous system hasn't downshifted in months.
Meanwhile, a hospital administrator rewrites protocols under fluorescent lights, her own clarity and energy running dangerously low.
This is the paradox we don't talk about enough: Those we trust to lead and heal are often leading from depletion.
Burnout Isn't Just a Statistic. It's a Signal.
Burnout in healthcare isn't breaking news—it's everywhere. A trending topic. A checklist item in leadership meetings. Easy to acknowledge, even easier to ignore. But it's not just a trend to talk about. It's a signal—one too many professionals are trained to dismiss.
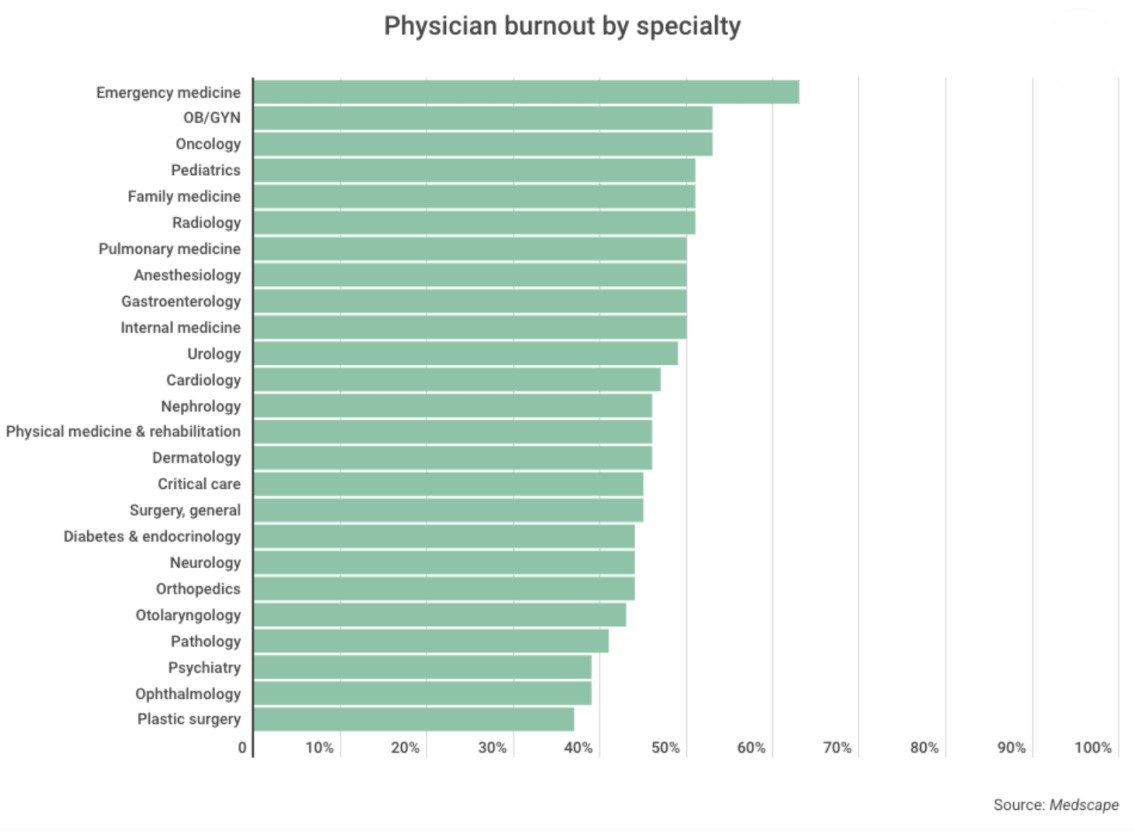
Emergency medicine leads with 63% burnout. OB-GYN and oncology follow at 53%. Over half of female physicians report it. These numbers don't just inform—they warn. Behind them are exhausted bodies, anxious minds, and nervous systems stuck in survival mode.
 A pediatrician I coach once said: "I can hold a sick baby in one arm and finish a chart with the other—but some days I come home and can't remember if I ate. My brain is full, but I feel empty."
She's not alone. 93% of healthcare workers report stress. 86% report anxiety. 76% report exhaustion. These aren't outliers—they're the atmosphere.
And the cost is real: increased turnover, diminished patient care, rising medical errors. Burnout doesn't stay personal. It becomes systemic.
Yes, the causes are complex—staffing, admin demands, shifting pressures. And yes, solutions are being offered. But here's what we're still missing:
We train for performance. We reward endurance. But we rarely teach leaders how to manage what matters most—their internal system.
And under pressure, that's what everything falls back on.
You don't rise to the level of your goals. You fall to the level of your internal system.
A pediatrician I coach once said: "I can hold a sick baby in one arm and finish a chart with the other—but some days I come home and can't remember if I ate. My brain is full, but I feel empty."
She's not alone. 93% of healthcare workers report stress. 86% report anxiety. 76% report exhaustion. These aren't outliers—they're the atmosphere.
And the cost is real: increased turnover, diminished patient care, rising medical errors. Burnout doesn't stay personal. It becomes systemic.
Yes, the causes are complex—staffing, admin demands, shifting pressures. And yes, solutions are being offered. But here's what we're still missing:
We train for performance. We reward endurance. But we rarely teach leaders how to manage what matters most—their internal system.
And under pressure, that's what everything falls back on.
You don't rise to the level of your goals. You fall to the level of your internal system.
Leadership Has Evolved—But Not Far Enough
Healthcare leadership has evolved. We've seen a growing emphasis on systems thinking, collaboration, and interprofessional coordination. But even with these advances, most leadership development still revolves around the outer game—strategy, productivity, decision frameworks.
What's missing is the inner game: the leader's ability to self-regulate, stay centered in complexity, and respond rather than react under pressure.
We've seen this gap before—the disconnect between external planning and the internal systems leaders rely on to think, decide, and adapt in real time.
History has shown us that the best strategies can fall apart when leaders don't build the internal flexibility to adapt under pressure. After 9/11, then–CIA Director George Tenet described the intelligence community's failure to anticipate the attacks as "a colossal failure of imagination"—a breakdown not of data, but of mental agility.
Today, this gap is showing up in healthcare. We've got strategies in place, but decision-making falters when pressure mounts. Leaders know what to do, but in the heat of the moment, their clarity, composure, and creativity slip away.
This isn't just a performance problem—it's an internal systems problem. Without developing the mental flexibility to manage energy, emotion, and attention under pressure, even the most well-resourced systems can break down.
If we continue developing leadership from the outside in, we'll miss the critical opportunity to build internal systems that support resilience, clarity, and presence when it matters most.
Self-Leadership as Infrastructure
In healthcare, self-leadership isn't just a personal asset—it's a leadership imperative. It fuels our ability to think clearly, communicate effectively, and respond intentionally in environments that rarely slow down.
At its core, self-leadership is the ability to manage one's internal state with precision and purpose, not when things are easy but precisely when they aren't. This is more than theory; it's measurable. A 2023 study in the Journal of Healthcare Management found that leaders trained in emotional regulation techniques demonstrated a 31% improvement in team psychological safety scores and a 17% reduction in reported medical errors over six months.
 Dr. Michael Frisina's seminal work, "Leading with Your Upper Brain," provides a neuroscience-based framework that supports these outcomes. His research demonstrates how leaders who operate from the "upper brain"—the prefrontal cortex responsible for executive function and emotional regulation—create environments characterized by psychological safety, improved communication, and enhanced decision-making. As Frisina notes, when healthcare leaders develop these self-regulation capabilities, they transform not just their own effectiveness but the entire organizational culture around them.
And critically, self-leadership isn't just for executives. It's for anyone who leads people, projects, or patients—including those who never saw themselves as leaders at all.
Dr. Michael Frisina's seminal work, "Leading with Your Upper Brain," provides a neuroscience-based framework that supports these outcomes. His research demonstrates how leaders who operate from the "upper brain"—the prefrontal cortex responsible for executive function and emotional regulation—create environments characterized by psychological safety, improved communication, and enhanced decision-making. As Frisina notes, when healthcare leaders develop these self-regulation capabilities, they transform not just their own effectiveness but the entire organizational culture around them.
And critically, self-leadership isn't just for executives. It's for anyone who leads people, projects, or patients—including those who never saw themselves as leaders at all.
A Framework for Developing Internal Leadership Capacity
To cultivate self-leadership, we propose a tripartite model focused on three executive competencies:
- Cognitive Agility: The capacity to maintain mental clarity, engage in metacognitive awareness, and strategically direct attention resources during periods of acute and chronic stress.
- Affective Intelligence: The intentional regulation of emotional states—not through suppression, but through calibrated modulation—utilizing evidence-based techniques to sustain intrinsic motivation and resilience during system-wide pressure.
- Deliberate Response Integration: The ability to make value-aligned decisions under pressure—responding with clarity, not reactivity—even when systems are in flux.
These competencies form an integrated system, each reinforcing the others to support sustainable, human-centered performance.
"In healthcare, the quality of our leadership directly impacts the quality of care we provide. Self-leadership is the foundation upon which all other leadership functions rest," explains a Chief of Emergency Medicine I recently worked with. She implemented daily mindfulness practices with her leadership team based on these principles. Within months, her department saw measurable improvements in communication effectiveness and staff retention. "The shift wasn't in what we did," she notes, "but in how we showed up to do it."
These competencies don't develop overnight, but they can be systematically strengthened through evidence-based protocols, neuropsychological techniques, and structured reflection. Even five minutes of deliberate practice each day creates measurable improvements over time.
This Isn't Optional
The ripple effects of self-leadership extend beyond individual resilience. Leaders who operate from a regulated internal state elevate the people around them. They create teams that communicate more effectively, recover more efficiently, and perform more consistently, especially when it counts most.
This is what Dr. Frisina refers to as the "contagion effect" of upper-brain leadership. Presence isn't just personal—it's organizational.
In high-stakes healthcare environments, this kind of leadership isn't optional. It's a non-negotiable requirement for long-term sustainability, patient safety, and clinical excellence.
During my time as an Army helicopter pilot, I witnessed firsthand how leaders who maintained internal regulation during crisis situations not only made better decisions but created an atmosphere of calm competence that enhanced team performance.
We saw this same phenomenon in action with Captain Chesley "Sully" Sullenberger during the Miracle on the Hudson. When both engines failed mid-flight, it wasn't just skill that saved 155 lives—it was internal mastery. As Sullenberger later said, his ability to stay composed was no accident. It came from "making small, regular deposits throughout my life of education, training, and experience"—the kind of deposits that allow for a life-saving withdrawal when everything is on the line.
Self-leadership isn't extra. It's infrastructure. If we want to move the metrics that matter—outcomes, retention, well-being—we must start from within. Modern healthcare can't afford leaders who only lead from the outside in. The future belongs to those who lead from the inside out.
An Invitation to Go Deeper
We've trained to lead care. We've trained to lead teams. But have we trained to lead ourselves?
Self-leadership asks us to go deeper: to find clarity when chaos surrounds us. To stay grounded when the storm swirls. To stay connected when the pressure is at its peak.
This isn't a distant, abstract idea—it's the difference between surviving and thriving in healthcare. It's the shift that transforms the way we lead and the way we heal. It's the leadership that our teams—our patients—need most.
Imagine a healthcare environment where every leader operates with clarity, resilience, and purpose. Where the ripple effect of self-leadership fosters psychological safety, reduces errors, and elevates care. It's possible. And it starts with you.
This September, healthcare leaders from across the country will gather at the ABQAURP conference to explore this new frontier of leadership. The session, The Self-Leadership Framework: A New Model for Influence and Impact, will offer science-backed strategies to optimize decision-making, emotional regulation, and influence, especially when the pressure is highest. This isn't just an opportunity—it's a call to evolve. Will you answer it? Register today at ABQAURP.org/AnnualConference. Your leadership—and the future of healthcare—depends on it.
About the Author
Traci Fisher is the CEO of The Wellness Coach and the creator of The Healthy Leader Operating System™. She partners with healthcare leaders to build sustainable leadership from the inside out—using evidence-based self-regulation tools to improve clarity, connection, and resilience under pressure.
A West Point graduate and former Army helicopter pilot, Traci blends military precision with neuroscience and behavior-change expertise to help leaders navigate complexity with presence and purpose. Learn more at www.thewellness.coach.
REFERENCES
Medscape. (2024). Physician Burnout & Depression Report 2024. Retrieved from https://www.medscape.com/slideshow/2024-lifestyle-burnout-6016058
Sullenberger, C. B. (2009). Leadership lessons from Captain "Sully" Sullenberger. Retrieved from https://chiefexecutive.net/4-things-ceos-can-learn-captain-chesley-burnett-sully-sullenberger/
Frisina, M. E. (2019). Leading with Your Upper Brain: How to Create the Behaviors That Drive Success in Healthcare. Chicago, IL: Health Administration Press.